Cirrhosis of the liver
Key facts
- Cirrhosis is liver scarring, which impairs its function and can be very serious.
- Symptoms of cirrhosis are appetite loss, weight loss, bruises, yellow skin and confusion.
- Causes of cirrhosis include hepatitis, long-term alcohol abuse and fatty liver.
- Diagnosis is by physical examination and blood tests, scans or liver biopsy.
- Cirrhosis can’t be cured, but you can control symptoms with a healthy lifestyle.
What is cirrhosis?
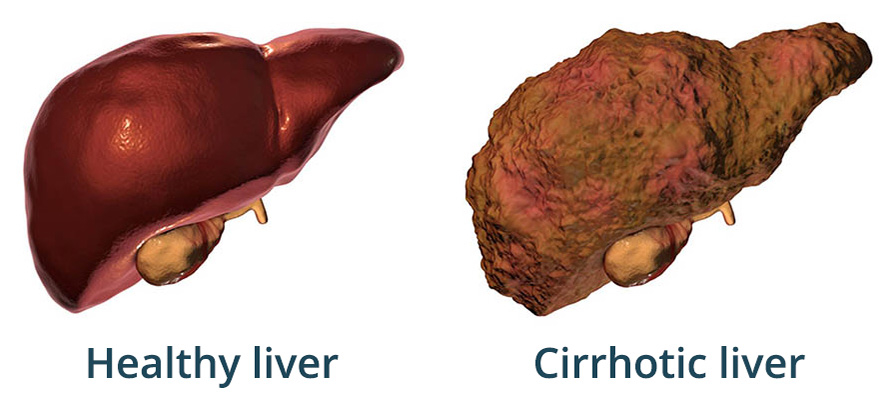
Cirrhosis is permanent scarring of the liver caused by many liver diseases and conditions, such as hepatitis and alcohol abuse.
Your liver is a vital organ that has many important functions for keeping your body healthy, including:
- removing toxins from your blood
- storing vitamins, extra glucose and iron
- making and breaking down hormones and proteins
When your liver is permanently damaged, scar tissue replaces healthy tissue. This is cirrhosis. It usually develops slowly over many years and can eventually stop your liver from working properly.
Although there is no cure for cirrhosis, early diagnosis and treatment can stop or delay its progress. This can lower the damage and reduce your chance of developing complications.
If cirrhosis becomes very serious it causes your liver to fail and can be life-threatening.
Aboriginal and/or Torres Strait Islander people have a higher risk of liver disease than non-Indigenous Australians.
What are the symptoms of cirrhosis?
Not everyone has the same symptoms. They can include:
- loss of appetite or weight loss
- weakness
- increased sensitivity to medicines and drugs
- confusion
- drowsiness
- slurred speech
They can also include visible symptoms such as:
- bruising and bleeding easily
- jaundice (yellowing of your skin and whites of your eyes)
- ascites (fluid build-up in your abdomen)
- skin conditions, such as liver spots (also called solar lentigo), spider veins and rashes
- oedema (swelling in legs)
- red palms of your hands
Some of these symptoms can be serious.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes cirrhosis?
Anything that damages your liver can cause cirrhosis, but the most common causes are:
- hepatitis B or hepatitis C infections
- drinking too much alcohol over many years (chronic alcohol dependence)
- being overweight or having too much fat in the liver (fatty liver), which is linked to obesity and diabetes
Less common causes of cirrhosis are:
- autoimmune liver disease, such as primary biliary cholangitis (previously known as primary biliary cirrhosis)
- inherited liver diseases, such as haemochromatosis
When should I see my doctor?
It’s important to speak to your doctor if you are experiencing symptoms of cirrhosis, especially if you have risk factors for liver problems.
When to seek urgent care
If your doctor has diagnosed you with cirrhosis, seek urgent medical attention if you experience:
- new or worsening jaundice (yellowing of your skin or the whites of your eyes)
- blood in your stools, or stools that are black and tar-like
- fresh blood in your vomit, or vomit that looks like ‘coffee grounds’
- confusion
- fever
Watch this video called Your Healthcare Team, from the Liver Foundation.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is cirrhosis diagnosed?
If your doctor suspects you have cirrhosis, they will ask about your symptoms, examine you and refer you for tests.
Tests that help to diagnose cirrhosis include:
- blood tests, including liver function tests
- urine (wee) tests
- imaging tests, including ultrasound, CT scans or MRI scans
- liver biopsy (taking a small piece of tissue from your liver to be tested)
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is cirrhosis treated?
Treatment depends on the cause and stage of your cirrhosis.
Your doctor may advise that you:
- stop drinking alcohol permanently
- lose weight, if you are overweight
- maintain a healthy diet
- stay physically active
- take medicines prescribed to treat any underlying causes (such as hepatitis C, autoimmune disease, inherited liver disease)
Support groups like Alcoholics Anonymous Australia and Alcohol and Drug Foundation are available to help you reduce or stop drinking.
Very advanced cirrhosis can cause the liver to fail. In this case, a liver transplant is the only treatment option.
Can cirrhosis be prevented?
To help reduce your chance of developing liver diseases including cirrhosis:
- eat a balanced diet
- take care with how much alcohol you drink, and know your limit
- exercise regularly
You can reduce the risk of fatty liver by:
- exercising regularly
- eating healthily
- losing weight
Hepatitis infections can increase your chance of developing liver problems. You can reduce your chance of catching hepatitis by:
- getting vaccinated against hepatitis B
- practising safe sex
- use safe needle practices (for example, don’t share needles)
Lower your chance of getting infections by washing your hands properly and making sure your vaccinations are up to date.
Before using any over-the-counter medicines, talk to your doctor or pharmacist and let them know you have liver disease.
What are the complications of cirrhosis?
Without treatment, cirrhosis of the liver can lead to serious and life-threatening problems including:
- primary liver cancer — hepatocellular carcinoma is the most common type of cancer caused by cirrhosis
- liver failure
- fluid build-up in the abdomen, which can become infected
- osteoporosis (brittle bones)
- encephalopathy — which can cause changes in mood and behaviour, confusion or coma
Resources and support
For more information and support about cirrhosis, try these resources:
- Hepatitis Australia provides a fact sheet about cirrhosis. Call the National Hepatitis Infoline: 1800 437 222 (1800 HEP ABC) for confidential, free access to hepatitis information and support.
- The Liver Foundation provides a wide range of resources and support related to liver health and practical tips for living well with liver disease. Call the Liver Foundation's free support line on 1800 841 118 to speak to a liver nurse.
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with you 24 hours a day, 7 days a week.
Languages other than English
Health Translations has resources about liver health and liver disease available in multiple languages.
Information for Aboriginal and/or Torres Strait Islander peoples
LiverWELL works with Aboriginal and Torres Strait Islander Communities to improve access to support services for testing and treatment. Call the LiverLine on 1800 703 003.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2025













