Ovarian cancer
Key facts
- Ovarian cancer does not usually cause noticeable symptoms in its early stages and is often diagnosed at an advanced stage.
- Ovarian cancer is usually treated with surgery, however chemotherapy, radiotherapy and targeted therapy may also be used.
- Ovarian cancer is more common in older females and those with a family history of cancer of the reproductive organs.
- If you have risk factors for ovarian cancer, you may wish to discuss preventative treatment with your doctor.
What is ovarian cancer?
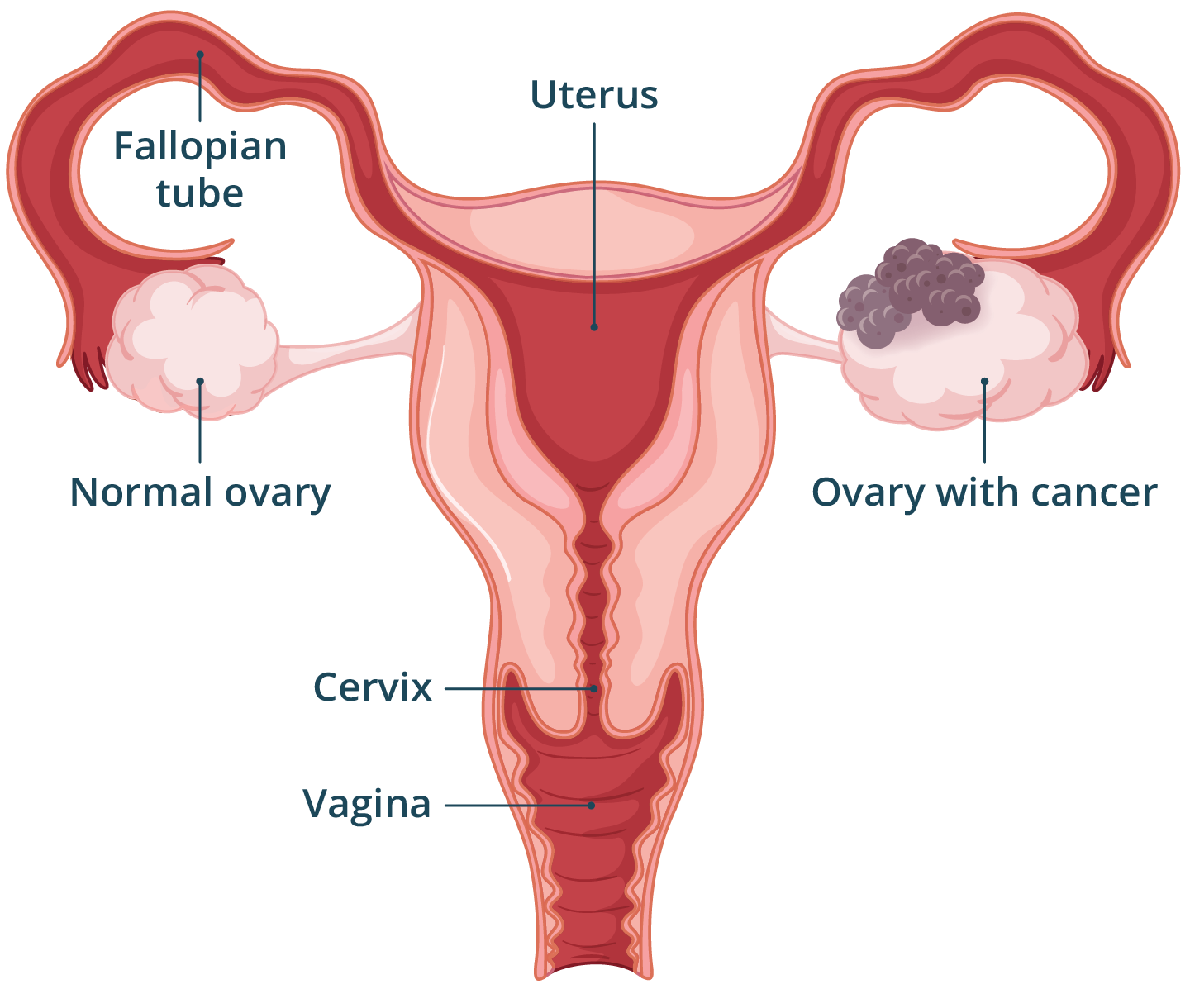
Ovarian cancer is when cells in your ovary, fallopian tube or the peritoneum — the outer covering of the abdominal and pelvic organs — grow in an abnormal and uncontrolled way.
There are 3 main types of ovarian cancer. The type of cancer depends on which ovarian cells are affected.
- Epithelial tumours affect the surface cells of the ovary, fallopian tube or peritoneum. They make up about 9 out of 10 ovarian cancers and there are different subtypes. They usually affect females over 60 years of age.
- Stromal cell tumours or sex cord-stromal tumours that affect the hormone-producing cells in the ovary. They make up less than 8 in every 100 cases of ovarian cancer. They usually occur in females aged 40 to 60 years.
- Germ cell tumours affect the ovarian cells that develop into eggs, usually in females under 40 years of age. They make up about 4 in every 100 cases of ovarian cancer.
Ovarian cancer is staged according to the International Federation of Gynecology and Obstetrics (FIGO) system. There are 4 stages:
- Stage I: cancer found in one or both ovaries or in the fallopian tubes.
- Stage II: cancer in one or both ovaries or fallopian tubes as well as other organs in the pelvis, such as the uterus, bladder or bowel.
- Stage III: cancer in one or both ovaries or fallopian tubes that has spread to the lining of the abdomen (peritoneum) or to lymph nodes.
- Stage IV: cancer has spread outside the abdomen to other organs such as lungs or liver.
What are the symptoms of ovarian cancer?
Ovarian cancer does not usually cause symptoms in its early stages. When it does cause symptoms, they can be similar to other conditions. If you have any of the symptoms and they are new or continue for more than a few weeks, you should talk with your doctor.
The most common symptoms of ovarian cancer include:
- feeling bloated
- back, abdominal or pelvic pain
- feeling full after eating small amounts
- urinary changes, such as difficulty urinating or needing to urinate urgently
Other symptoms may include:
- changes in bowel habits
- unexplained weight loss or gain
- fatigue
- nausea or indigestion
- pain when having sex
- vaginal bleeding between periods, after menopause or after sex
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes ovarian cancer?
The cause of ovarian cancer is unknown. However, there are factors that have been shown to affect your chance of developing ovarian cancer.
Risk factors that may increase your risk of developing cancer include:
- older age – ovarian cancer is more common if you are over 50 years
- family history of certain cancers in close relatives, including ovarian, breast, colorectal and endometrial
- having certain faulty genes such as BRCA (more common in people of Ashkenazi Jewish ancestry) or Lynch syndrome
- being overweight
- smoking
- endometriosis
- if you’ve never been pregnant
Factors that may reduce your risk of developing ovarian cancer include:
- breastfeeding
- taking the oral contraceptive pill ('the pill') — especially if you’ve taken the pill for more than 5 years
- having your fallopian tubes removed
If you are concerned about your risk of ovarian cancer, see your doctor for more information and advice.
What’s your risk?
Check your cancer risk with Cancer Australia’s calculator.
When should I see my doctor?
Symptoms of cancer of the ovaries are common to other conditions, so having symptoms does not always mean you have cancer. If you notice new symptoms, or if they are severe, or if they continue for more than a few weeks, you should see your doctor.
You may find it helpful to track how often you have symptoms and how severe they are using Ovarian Cancer Australia's symptom diary and take this information with you to your doctor.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is ovarian cancer diagnosed?
If you or your doctor are concerned that you might have ovarian cancer, you will have a physical examination as well as tests and scans. If a tumour is found, you will need a biopsy to confirm it is a cancer.
Physical examination
Your GP or specialist doctor will perform a physical examination, including a pelvic examination, to look for signs of cancer.
A pelvic examination may involve your doctor looking inside your vagina with a medical tool called a speculum.
Your doctor may also check your uterus and ovaries for any lumps by placing 2 fingers inside your vagina, while feeling your abdomen with their other hand. Your doctor may perform a digital rectal examination by placing a gloved finger into your anus and rectum to check for any lump or masses. These examinations can be uncomfortable but should not be painful.
Blood tests and imaging
Your doctor may refer you for blood tests to check your general health and your kidney and liver function. In some cases, your doctor may also check your blood for a marker called CA-125 that is sometimes higher in ovarian cancer.
Your doctor may refer you for scans to check the size and location of the ovarian cancer and to see if the cancer has spread.
These may include:
- pelvic ultrasounds
- CT scans
- PET scans
- MRI scans
Biopsy
Ovarian cancer can only be diagnosed for certain with a biopsy. This involves taking a sample of the ovary or tumour and having it checked by a specialist doctor (pathologist) under a microscope. In most cases, a biopsy is taken during surgery.
If you are diagnosed with ovarian cancer, your doctor will consider how far it has spread and how fast the cancer cells are growing to determine its stage. This process helps your medical team decide on the best treatment plan for you.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is ovarian cancer treated?
The type of treatment your doctor recommends will depend on many factors, including:
- the type and stage of your cancer
- your age
- your general health
- if your cancer is related to a particular gene
- if you plan to have children in the future
Most cases of ovarian cancer are treated with surgery and or chemotherapy. Surgery for ovarian cancer is usually complex and is performed by a specialist team in a hospital with experience treating reproductive cancers. The exact type of surgery will depend on how far the cancer has spread. It may involve removing your ovaries, uterus, fallopian tubes, cervix, and part of your bowel or bladder.
Your doctor may recommend other treatments in addition to surgery, or instead of surgery if you are not well enough for an operation. These treatments may include chemotherapy, radiotherapy, and/or targeted therapies. Your doctor will discuss with you the benefits, risks and side effects of each of these treatments in your situation.
Can ovarian cancer be prevented?
Some healthy females who are considered at high risk of developing ovarian cancer may choose to have their ovaries and fallopian tubes removed to reduce their risk. People at a higher risk of developing ovarian cancer include those who have a strong family history of ovarian cancer and those with a genetic mutation that increases their risk of developing ovarian cancer.
If you are concerned about your own risk, you may wish to discuss your options with your doctor.
What are the complications of ovarian cancer?
Ovarian cancer and its treatment can lead to several symptoms and problems. You may experience any or none of these, depending on the type and stage of cancer and the treatment you are receiving.
Common problems may include:
- fatigue, especially if you are having chemotherapy or radiotherapy
- changes in your bowel habits
- fluid build-up in your abdomen (ascites), lungs (pleural effusion) or limbs (lymphoedema)
If your ovaries are removed to treat ovarian cancer, you will go through menopause. This means your periods will stop and you may experience other menopause symptoms. Treatment for ovarian cancer may also impact your sexuality and self-esteem.
Many of the treatments used for ovarian cancer will affect your ability to have children. If having children is important to you, speak to your doctor about options for fertility preservation before starting cancer treatment.
Your medical team is very experienced at managing complications associated with ovarian cancer and treatment. They can give you advice about managing any side effects that you may be experiencing.
Resources and support
Receiving a diagnosis of cancer can be overwhelming. There are many organisations that can provide you with information and support:
- Call Ovarian Cancer Australia on 1300 660 334, between 9am and 5pm, to speak with an ovarian cancer nurse on their Support and Information Helpline.
- Call Cancer Council on 13 11 20 between 9am and 5pm Monday to Friday. Cancer Council offers confidential information and support services for people living with cancer, their friends, families and healthcare professionals.
- The Cancer Australia website offers a publication-and-resource library which can be accessed for free. The library contains factsheets about cancer, evidence-based resources, cancer screening programs and cancer treatment.
- The Peter MacCallum Cancer Centre provides information about research, discovery and clinical trials, and access to the latest significant peer-reviewed publications.
Other languages
Do you speak a language other than English?
- Cancer Council South Australia has information in many different community languages.
- General information from NSW Health about cancer is available online in many community languages.
Aboriginal and Torres Strait Islanders
Cancer Council NSW provides information all about cancer for Aboriginal and/or Torres Strait Islander peoples.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2023
















