Endometrial cancer
Key facts
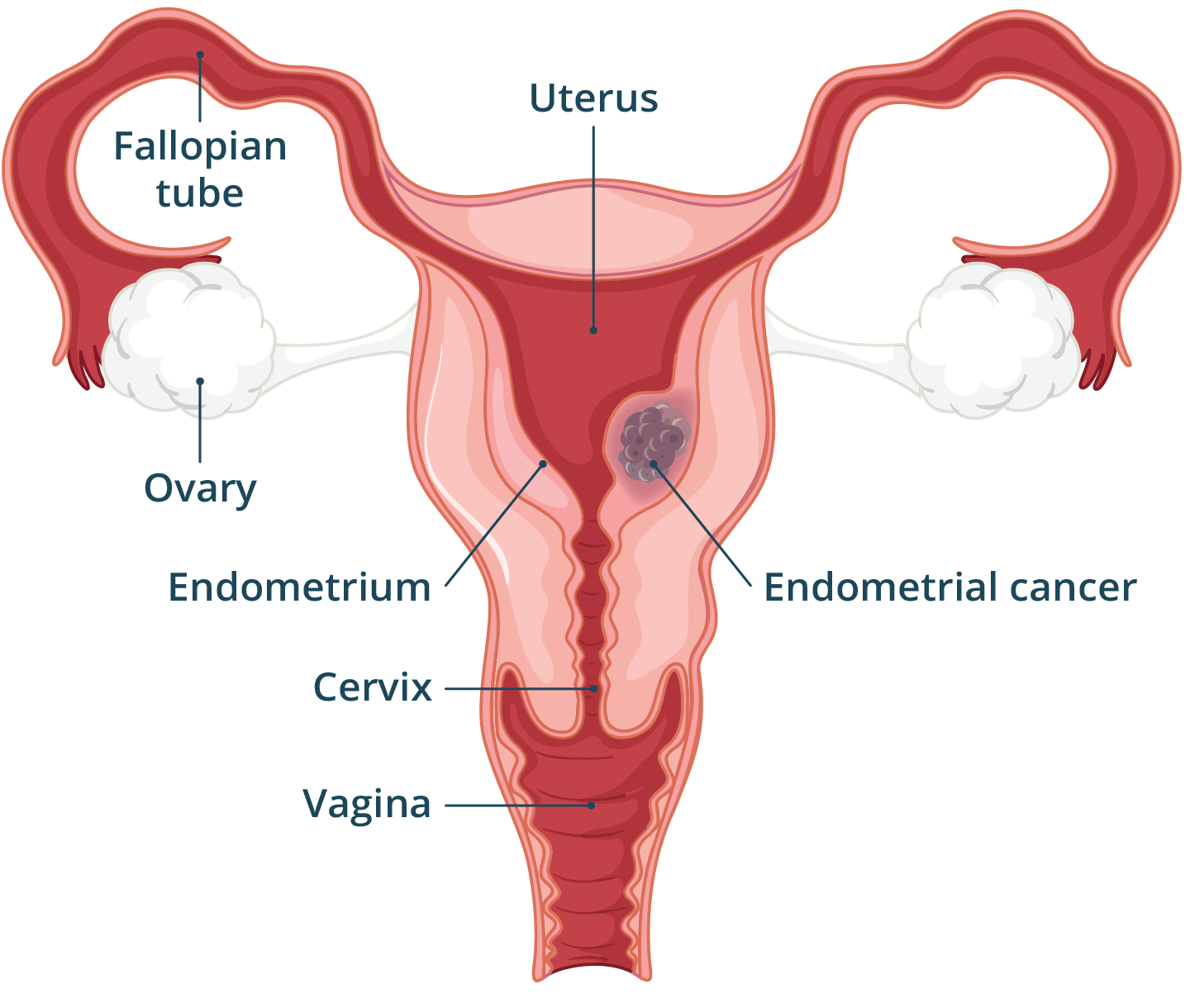
- Endometrial cancer occurs when the cells lining the uterus (endometrium) grow in an abnormal and uncontrolled way.
- The most common symptom of endometrial cancer is abnormal vaginal bleeding.
- Other symptoms include watery vaginal discharge, unexplained weight loss, difficulty urinating and abdominal (tummy) pain.
- Treatment options include surgery (such as hysterectomy), radiotherapy, chemotherapy and hormone therapy.
- If you have abnormal or unexpected vaginal bleeding, see your doctor so they can check the cause and make a diagnosis.
What is endometrial cancer?
Endometrial cancer develops when the cells lining the uterus — known as the endometrium — grow in an abnormal, uncontrolled way. Endometrial cancer is the most common gynaecological (women’s health) cancer in Australia.
Endometrial cancer is more common in females over 50 years of age who have gone through menopause. Younger females, transgender males and intersex people can also develop endometrial cancer.
Endometrial cancer is categorised into 4 stages, which can be broken down in to substages.
- Stage I: cancer is only in the uterus.
- Stage II: cancer has spread from the uterus to the cervix.
- Stage III: cancer has spread beyond the uterus and cervix, into the ovaries, fallopian tubes, vagina or lymph nodes of the pelvis or abdomen.
- Stage IV: cancer has spread further to the urinary bladder, bowel, rectum, abdomen, bones, lungs or lymph nodes of the groin.
What are the symptoms of endometrial cancer?
A common early symptom of endometrial cancer is abnormal vaginal bleeding, especially bleeding after menopause. If you are still having your period other symptoms include, bleeding between periods, constant bleeding, or a change in your periods including heavier periods.
Other symptoms include:
- a watery vaginal discharge (this may have an unpleasant smell)
- unexplained weight loss
- difficulty urinating (weeing)
- a change in bowel (pooing) habits
- abdominal (tummy) pain
If you have one or more of these symptoms, it doesn't necessarily mean you have endometrial cancer. These symptoms can occur for many other reasons. However, it's important to see a doctor to check.
What’s your risk?
Check your cancer risk with Cancer Australia’s calculator.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
When should I see my doctor?
If you notice any of the symptoms of endometrial cancer including abnormal vaginal bleeding, it is important to see your doctor. These symptoms are common and don’t necessarily mean you have cancer. However, it’s best to have it checked. You can ask to see a female doctor if you prefer.
Before your appointment, you can write a list of questions. This will help you to get more out of the time with the health professional. Use the healthdirect Question Builder tool. You can print it out or email so it's convenient for you to take to your appointment.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
What causes endometrial cancer?
The cause of endometrial cancer is unclear, but there are known risk factors. Some of the risk can be reduced by making changes to your lifestyle.
Risk factors related to your general health include if you:
- are living with overweight or obesity
- have high blood pressure (hypertension)
- have diabetes
- are over 50 years of age and have gone through menopause
- take the medicine tamoxifen (for breast cancer)
- have Lynch syndrome (known as hereditary non-polyposis colorectal cancer – HNPCC)
Risk factors related to your gynaecological health include if you:
- have endometrial hyperplasia (thickening of the lining of the uterus)
- had periods before the age of 12 or menopause after age 55
- take an oestrogen menopause hormone therapy with no progesterone
- have never been pregnant
- had had pelvic radiotherapy (to treat another cancer)
- have a tumour in one of your ovaries
- have polycystic ovary syndrome (PCOS)
How is endometrial cancer diagnosed?
If you have symptoms that might be caused by endometrial cancer, your doctor will start by asking you questions about your symptoms, your health and any history of cancer in your family.
As well as doing a general examination, your doctor will do a pelvic examination. This includes using a medical tool called a speculum to look inside your vagina, similar to doing a cervical screening. They will also feel your uterus by placing 2 fingers inside your vagina and their other hand on your abdomen. You can ask for a nurse or support person to be present during this examination.
Your doctor will also refer you for blood test and a pelvic ultrasound to take images of your uterus, endometrium, cervix and ovaries. Remember, you can ask to see a female health professional if you would prefer.
Your GP may do some of the initial tests, or they may refer you to a gynaecologist or gynaecological oncologist.
To confirm endometrial cancer you will need an endometrial biopsy. A small sample of cells is collected and checked under the microscope for cancer cells. Sometimes this can be done in a gynaecology clinic with a very thin tube, called a pipelle, inserted through your cervix. You can take some pain relief medicine before the biopsy to make it more comfortable — ask your doctor for a recommendation. If your doctor was unable to get enough cells to confirm a diagnosis, you may need another biopsy.
Another way to collect an endometrial biopsy is to have a hysterectomy, dilatation and curettage (‘D&C’). This is usually done in a day surgery clinic under anaesthetic so you don’t feel the procedure. You may have some crampy period-like pain and light bleeding for a few days afterwards.
You may also need a CT, MRI or PET scan.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is endometrial cancer treated?
If tests confirm endometrial cancer, your specialist will discuss treatment options with you. Often surgery is the only treatment you will need. Your doctor may recommend radiation therapy, chemotherapy or hormone therapy if your cancer has spread from the uterus.
Surgery
If your cancer is diagnosed early, surgery may be the only treatment you need.
Your doctor may discuss the need for a:
- total hysterectomy (an operation to remove your uterus and cervix)
- bilateral salpingectomy (removal of both fallopian tubes)
- bilateral ovariectomy (removal of both ovaries)
Depending on your cancer, you may be advised to also have your pelvic lymph nodes removed, known as a lymphadenectomy.
Radiotherapy
Radiotherapy or radiation therapy, uses x-ray beams to kill or damage cancer cells.
Radiotherapy is often used after surgery to reduce the risk of your cancer coming back. This is so they cannot grow, multiply or spread, while limiting damage to healthy organs of the body.
Radiotherapy may be external (when you lie near a machine that aims x-rays at your cancer), or internal (also known as brachytherapy, where a small radioactive device is placed inside your body for a few minutes).
Hormone therapy
Hormones such as oestrogen and progesterone, occur naturally in the body, and have many health functions. This includes controlling the growth and activity of cells. Sometimes a cancer uses the body’s own hormones to grow. These are called hormone-sensitive cancers, and they may be treated with hormone therapy.
Sometimes, your doctor will recommend hormone therapy in endometrial cancer if surgery hasn’t been done. For example in a you have early-stage cancer and want to have children in the future or if you are too unwell for surgery.
The therapy can be taken as tablets, or if you have not had a hysterectomy, by using a hormone-releasing intrauterine device (IUD) which is placed in your uterus by your doctor.
Chemotherapy
Chemotherapy uses medicines to kill or slow the growth of cancer cells, while aiming to cause minimal damage to healthy cells.
If you do need chemotherapy, you will need the medicines directly into your vein (known as IV). You will need several treatments, called cycles, over weeks or months. Usually, you can have treatment as an outpatient and you won’t need to stay in hospital overnight.
Can endometrial cancer be prevented?
There is no way to ensure you won’t get endometrial cancer. You can reduce some of your risk factors such as by maintaining a healthy weight.
The use of combined oral contraceptives ('the pill') for at least 5 years will lower your chance of developing endometrial cancer. If you are taking menopausal hormone therapy (also known as hormone replacement therapy, or HRT) and still have your uterus, your doctor will prescribe progesterone therapy as well as oestrogen replacement. Be sure to take your medicines exactly as your doctor prescribes.
If you have an increased risk of endometrial cancer, you may consider a risk-reducing hysterectomy. This includes if you have a condition known as atypical endometrial hyperplasia or a genetic condition such as Lynch syndrome. If you are considering this, you should discuss the risks and benefits of this approach with medical specialists in this area, such as at a familial cancer clinic.
What are the complications of endometrial cancer?
One of the possible complications of endometrial cancer is anaemia (a condition when you don’t have enough red blood cells or haemoglobin to carry enough oxygen in your blood). Complications of endometrial cancer mainly relate to the effects of cancer treatment. Surgery, chemotherapy, radiotherapy and hormonal therapy all have different side effects.
A cancer care nurse can help you understand these side effects and help you stay as comfortable as possible during your treatment.
Menopause
If you have not yet been through menopause, removing your ovaries and some other types of endometrial cancer treatment can bring on menopause suddenly. If you have had menopause some of the symptoms may come back.
Infertility
Having surgery to remove your uterus, or having radiation to your pelvis can prevent you from having a pregnancy. In certain cases, if you get an early diagnosis, you may be able to have it treated without removing your uterus. Speak with your health team to see if treatment to spare your ovaries and uterus is suitable for you.
Other complications
Other complications you may experience after treatment for endometrial cancer include:
- fatigue
- bowel and bladder changes
- lymphoedema
- vaginal vault prolapse
- changes to your sexuality how you feel about sex, how you respond sexually or physical changes such as vaginal dryness
Your medical team as well as social workers and support organisations can help you to manage these changes.
Resources and support
The Cancer Council provides the following information for cancer patients and their families:
- Support and services for Australians affected by cancer.
- Practical and financial assistance, help with transport, accommodation and financial costs and legal issues.
- Living with cancer resources that include emotional and practical information.
Other languages
Do you speak a language other than English?
- The Cancer Council has information for cancer patients and their families in community languages.
- General information about cancer is available from NSW Health in many community languages.
Aboriginal and Torres Strait Islanders
Cancer Council NSW provides information all about cancer for Aboriginal and/or Torres Strait Islander peoples.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2023















