Prolapsed uterus
Key facts
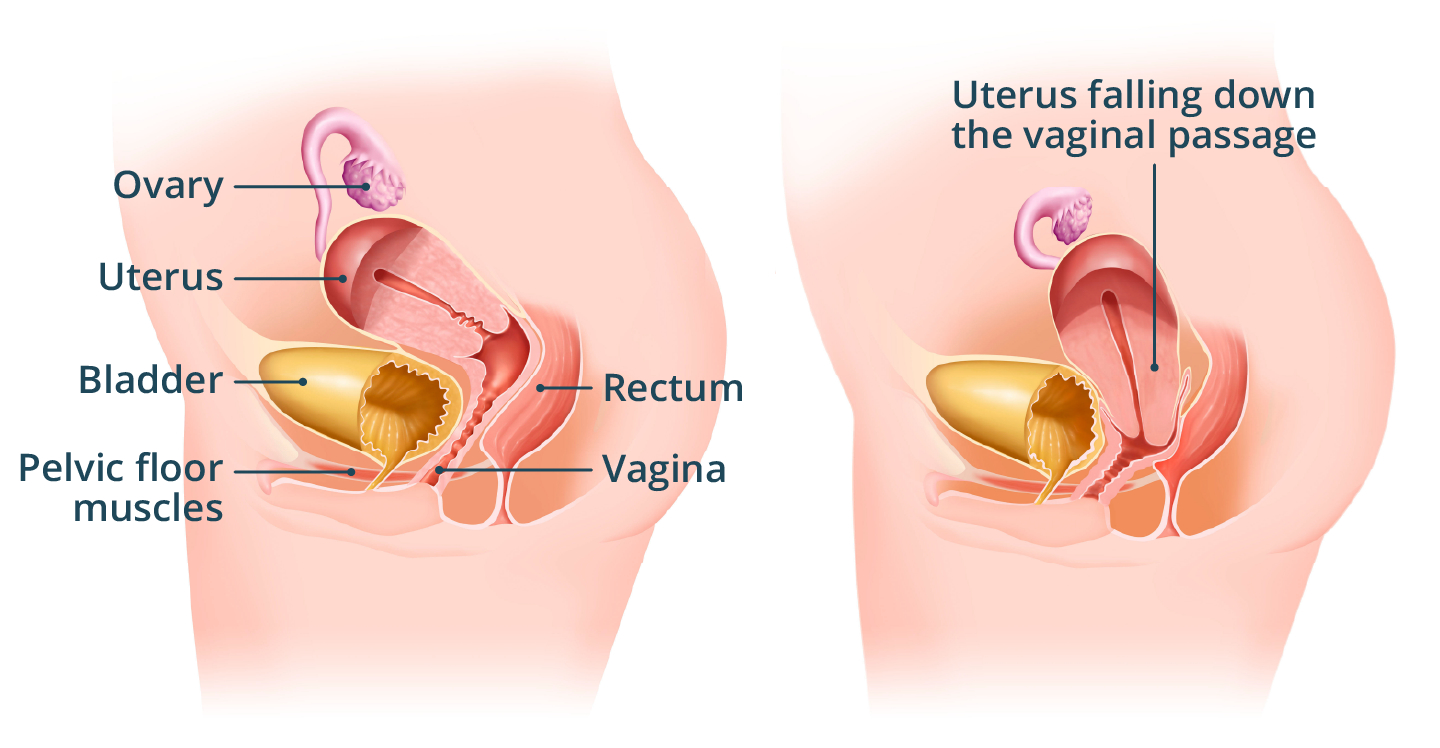
- A prolapsed uterus is when your uterus (womb) slowly drops down towards the opening of your vagina.
- A prolapse occurs when the muscle (pelvic floor) that holds your uterus in place becomes stretched or weak.
- A common symptom of a prolapsed uterus is a feeling of fullness in your vagina.
- Treatment will depend on the extent of the prolapse and how much it affects your daily life.
- Talk to your doctor about the different treatment options available.
What is a prolapsed uterus?
A prolapsed uterus occurs when your uterus (womb) slowly drops down towards the opening of your vagina. A prolapsed uterus is also called ‘uterine prolapse'.
This can happen when the tissues that hold your uterus in place are stretched or weakened.
A prolapsed uterus is most common in females going through menopause and soon after giving birth.
A prolapsed uterus will often get worse without treatment.
What are the symptoms of a prolapsed uterus?
Common symptoms of a prolapsed uterus include:
- a feeling of fullness or pressure inside your vagina
- a bulge, that you can see or feel, at the opening of your vagina
- a sense of heaviness in your pelvis or vagina
You may also:
- be unable to completely empty your bladder (wee) or bowel (poo) when going to the toilet
- have bladder or bowel urgency (needing to go to the toilet very suddenly)
- have incontinence (loss of bladder or bowel control)
- have urinary tract infections that keep coming back
- have pain during sex or less sensation during sex
Your symptoms may feel worse after standing or exercising. Your symptoms will often feel better after lying down.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes a prolapsed uterus?
Your pelvic organs (uterus, bladder and rectum) are usually held in place by the muscles and soft tissue in your pelvic floor. When your pelvic floor is stretched or weakened your pelvic organs can come out of place, which is called a prolapse.
A prolapsed uterus can happen when something puts pressure on your pelvic floor, such as:
- pregnancy and childbirth
- prolonged constipation, or regularly straining on the toilet
- repeated heavy lifting
- being overweight or obese
- having a chronic (ongoing) cough
You are more likely to have a prolapse after menopause or as you get older.
When should I see my doctor?
See your doctor if you have any symptoms of a prolapsed uterus, such as:
- a sensation of fullness inside your vagina
- incontinence (loss of bladder or bowel control)
- a lump in, or out of, your vagina
- pain during sex
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is a prolapsed uterus diagnosed?
Your doctor can diagnose a prolapsed uterus. They will ask about your symptoms and your health in general. They may also ask if they can do an internal vaginal examination. You can request a female doctor if that makes you feel more comfortable.
Find out more about your rights when having a vaginal examination.
You may also be asked to have some tests, like:
- an ultrasound scan
- a urine test
- urodynamic studies (to check your bladder function)
Your doctor may refer you to a gynaecologist. A gynaecologist is a doctor who specialises in female reproductive health.
Stages of uterine prolapse
Doctors use a grading system to describe how much of your uterus is pushed down into your vagina.
- Stage 1 — the uterus drops into the upper part of the vagina.
- Stage 2 — the uterus drops into the lower part of the vagina.
- Stage 3 — the uterus protrudes outside of the opening of the vagina.
- Stage 4 — the uterus slips completely outside the vagina.
In some people, the bladder and bowel can also prolapse.
- A cystocele is when your bladder bulges into the front of your vagina.
- A rectocele is when your rectum (lower part of your large bowel) bulges into the back of your vagina.
- A vaginal prolapse is any combination of a uterine prolapse, cystocele and rectocele.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is a prolapsed uterus treated?
Treatment will depend on the type of prolapse, and how much it affects your daily life.
Treatment options can include:
- lifestyle measures
- pelvic floor strengthening
- vaginal pessaries
- oestrogen cream
- surgery
Some of these treatments can be used in combination.
Talk with your doctor about the different treatment options. It's important to discuss the benefits and risks, so that you can make an informed decision.
Without treatment, your symptoms are likely to get worse. If your symptoms don’t affect your usual activities, you can choose not to have any treatment. You can always change your mind if your symptoms start to bother you.
Lifestyle measures
There are lifestyle measures that can help with a prolapsed uterus. You should:
- do regular physical activity
- avoid heavy lifting
- avoid high impact exercise
- eat high fibre foods and stay hydrated to prevent constipation
- maintain a healthy weight
- avoid smoking
It can take time for these lifestyle changes to work.
Pelvic floor muscle exercises
Strengthening your pelvic floor muscles and changing your daily activities can help if you have a mild prolapse.
Your doctor may refer you to a pelvic floor physiotherapist to help with pelvic floor muscle exercises. Your physiotherapist may also show you how to avoid straining and support your prolapse when going to the toilet.
Vaginal pessaries
You may be offered a device called a pessary. If you choose to use a pessary, a specialist doctor will fit it in your vagina. This supports your pelvic organs and can improve your prolapse symptoms. A pessary can be removed at any time.
Oestrogen cream
You can apply oestrogen cream to your vagina. It can help manage symptoms such as irritation of the skin and tissue around your prolapse.
Surgery
If you have a severe prolapse and your symptoms do not improve with other treatments, surgery may help.
Your doctor will talk with you about different surgical procedures to repair the prolapse. It's important to talk through all the options so you understand the risks and benefits.
What are the complications of a prolapsed uterus?
If you have a prolapsed uterus, it will often get worse without treatment. This can lead to complications such as:
- vaginal bleeding
- dyspareunia (pain during sexual activity)
- urinary retention (difficulty emptying your bladder)
- pelvic pain
- worsening of symptoms in future pregnancies
Talk with your doctor about the different treatment options available.
If you choose to have surgery for your prolapsed uterus, this can also cause complications.
Can a prolapsed uterus be prevented?
The best thing you can do to prevent a prolapsed uterus is to keep your pelvic floor muscles strong with specific exercises. You can have your exercises checked by a pelvic floor physiotherapist to make sure you are doing them correctly.
You should also:
- do regular physical activity
- avoid heavy lifting
- avoid high impact exercise
- maintain a healthy weight
- eat high fibre foods and stay hydrated to prevent constipation
Visit the Pelvic Floor First website from Continence Health Australia for more information about pelvic floor strengthening.
Resources and support
For more information on prolapsed uterus or bowel or bladder problems, visit:
- Jean Hailes for Women's Health
- Continence Health Australia — or call their helpline on 1800 33 00 66
You can call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with you 24 hours a day, 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2025














