Greater trochanteric pain syndrome (GTPS)
Key facts
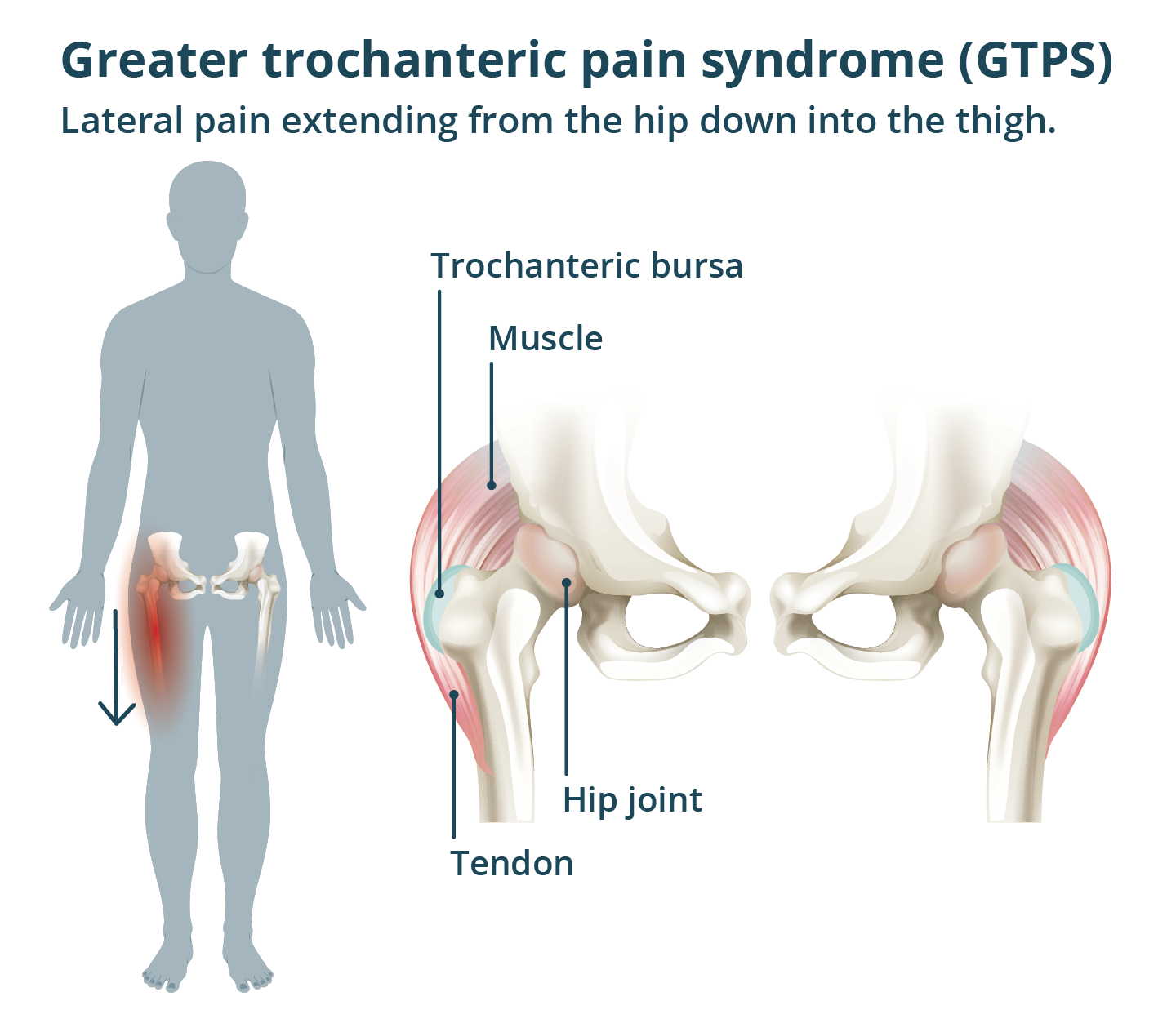
- Greater trochanteric pain syndrome (GTPS) is a condition that causes pain in the outside of your hip.
- It may cause pain in your hip, thigh or buttock area.
- GTPS can affect anyone, but it’s more common in females aged over 40 years.
- GTPS may start due to changes in your activity levels or for no specific reason.
- Exercise can help ease your symptoms and can also help to stop them from coming back.
What is greater trochanteric pain syndrome (GTPS)?
GTPS is a condition which causes pain in the outside of your hip. It can cause hip pain in one or both of your hips.
It happens when the tendons on the outside of your hip become irritated. These tendons attach the gluteal muscles in your bottom to the side of your hip.
You need your gluteal muscles and tendons for:
GTPS is also called lateral hip pain. In the past it was often called trochanteric bursitis, but this is a different condition.
GTPS can affect anyone. However, it’s more common in females and people aged between 40 and 60 years.
Nearly 1 in 5 people aged 50 to 79 years, report having GTPS.
The higher rate of GTPS in older females is caused by lower levels of sex hormones after menopause — this hormone helps protect the health of your tendons.
What are the symptoms of GTPS?
You may have some or all of these symptoms. Pain in your hip, thigh or bottom area when:
- standing on the affected leg
- going up stairs
- lifting your legs into bed
- sitting with your legs crossed
Your pain may get worse:
- when lying on your side
- with exercise such as walking or running
The area may also be sore when you touch it.
While these symptoms are like osteoarthritis, GTPS is not a type of arthritis.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes GTPS?
Your pain may start due to an increase in your activity levels, such as long-distance running. It can also start if you have been less active than normal. Often, GTPS starts for no reason.
Other things that may trigger GTPS are:
- living with overweight
- less strength and flexibility in your hip and bottom muscles
- sitting or standing in one position for too long
- having a sedentary lifestyle
- hormone changes
- an injury, such as a fall on your hip
When should I see my doctor?
See your doctor if you’ve followed the self-care advice below and your symptoms haven’t got better after 6 weeks.
You should also see your doctor if your symptoms are getting worse.
If you need to see your doctor but cannot wait for an appointment, you may be able to get treatment at a Medicare Urgent Care Clinic. Use the Service Finder to find your nearest one.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is GTPS diagnosed?
Your doctor will ask you about your symptoms and will examine your hips. They may also ask you to stand on one leg.
They may ask if you have difficulty putting on your socks and shoes. This helps to rule out osteoarthritis. People with GTPS can usually still put on their socks and shoes.
A diagnosis of GTPS does not need any tests.
Your doctor may arrange for you to have an ultrasound. This is to rule out other causes of your pain.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is GTPS treated?
It’s important to work out which activities are causing your pain. Changing these activities can help to improve your symptoms.
GTPS can take 6 to 12 months of rehabilitation to get better.
Self-care at home
Here are some helpful tips to improve your pain:
- Sit with your hips higher than knees.
- Don’t cross your legs when sitting.
- Don’t use low chairs.
- Stand evenly on both feet, do not lean on one leg.
- Try to keep active.
- Lose weight if you are living with obesity.
- Stay working, even if you have to change your duties.
At night:
- Do not lie on your sore hip.
- When lying on your side, put a pillow under your top leg.
- Sleep on your back when you can and put a pillow under your knees. The pillow helps to keep your legs in line with your hip joints.
Exercise
Your doctor or physiotherapist can work with you to create an exercise program. Most often this will include strength training that targets your gluteal muscles.
Aim to slowly increase your exercise over time. This lets your tendons and muscles become stronger. This will help to ease your pain. It will also help to stop your symptoms from coming back.
It’s important to keep exercising, even if you need to take pain-relief medicines or have some pain.
If your pain stays under 5 out of 10 and goes away in a day, the exercise is suitable for you. Exercise should not make your existing pain worse.
Your physiotherapist may also suggest:
- massage
- stretching
- heat treatments
It’s normal to have flare ups during recovery. If this happens, it may be best to do less exercise or rest for a few days before starting again.
Medicines for GTPS
You may want to take pain-relief medicines. You can use either paracetamol or an anti-inflammatory medicine (NSAIDs) such as ibuprofen. These can help you move more easily, which can help you get better.
If your pain is very bad, your doctor may suggest that you have a corticosteroid injection. This can ease your pain and help you start exercising.
Your doctor may suggest hormone replacement therapy (HRT) if:
- you’re post-menopausal
- your body mass index (BMI) is less than 25
What are the complications of GTPS?
GTPS causes chronic pain, which may lower your quality of life. It may cause you to have difficulty walking, going up and down stairs and getting into bed.
This may cause you to:
- do less physical activity — which will affect your health and fitness
- reduce your social activities due to the pain — this may affect your mental health
Treatments for GTPS can also cause complications. NSAIDs can cause stomach bleeding, especially in people who take blood thinners.
There can also be side effects from corticosteroid injections, such as:
- hyperglycaemia (high blood sugar) — particularly in people with diabetes
- infection
- weakening of tendons
Can GTPS be prevented?
You can help prevent greater trochanteric pain syndrome by exercising to strengthen your hip muscles to protect your tendons. Starting new exercises slowly to avoid hurting your hip.
A physiotherapist or exercise physiologist can create an exercise plan that is suitable for you.
You can help stop your GTPS symptoms coming back by exercising.
Resources and support
Musculoskeletal Health Australia (MHA) supports people with musculoskeletal conditions. You can call the BAM Helpline on 1800 263 265.
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2025









