Blood clots
If you or someone else is having trouble breathing, or if you have symptoms of stroke or heart attack, call triple zero (000) and ask for an ambulance.
Key facts
- Blood clotting can become a problem when it stops your blood from flowing properly.
- A blood clot that forms in a blood vessel is called a thrombus.
- Blood clots can cause different problems depending on where they are in your body.
What are blood clots?
Your blood can clot so that you don't lose too much blood if you are injured. But blood clotting can become a problem when it stops blood flow through your blood vessels.
A blood clot in a blood vessel is called a thrombus. It can be life-threatening if it's not treated quickly. Blood clots can lead to problems such as a:
If you think you may have a blood clot, see your doctor as soon as possible.
What are the symptoms of a blood clot?
Blood clots can cause different problems depending on where they are in your body.
The following conditions are caused by blood clots in blood vessels (arteries or veins) in different parts of the body.
Deep vein thrombosis (DVT)
A DVT is when a blood clot forms in one of the veins deep inside your body. DVTs mostly occur in your legs, but you can get a DVT anywhere in your body.
The most common symptoms of DVT are:
- pain and swelling in the affected area, usually your calf or thigh
- redness or discolouration of the skin near the blood clot
- more noticeable veins under the skin
Sometimes there are no symptoms.
Pulmonary embolism
If a blood clot travels from a deep vein to blood vessels in your lungs, it's called a pulmonary embolism.
Symptoms of a pulmonary embolism are:
- shortness of breath
- chest pain that may be worse with deep breaths
- coughing up blood
- rapid heartbeat or palpitations
- feeling lightheaded or fainting
A pulmonary embolism can be life-threatening.
If you think you may have a pulmonary embolism, go to the nearest emergency department or call triple zero (000) and ask for an ambulance.
Stroke
A blood clot in blood vessels in your brain can cause a stroke.
Symptoms of a stroke can include:
- weakness or drooping in your face, arm or leg
- difficulty speaking or understanding
- dizziness or loss of balance
- blurred vision
- difficulty swallowing
If you or someone else has signs of stroke, no matter how long they last, call triple zero (000) immediately and ask for an ambulance.
Heart attack
A blood clot in the blood vessels that supply your heart (coronary arteries) can lead to a heart attack.
Symptoms of a heart attack can include:
- chest pain or discomfort (it may feel like your chest is being pressed or squeezed by a heavy object)
- shortness of breath
- feeling weak
- nausea
- a cold sweat
- feeling anxious
- feeling dizzy or lightheaded
If you have any of these symptoms, or if they get worse quickly or last longer than 10 minutes, call triple zero (000) and ask for an ambulance.
What causes blood clots?
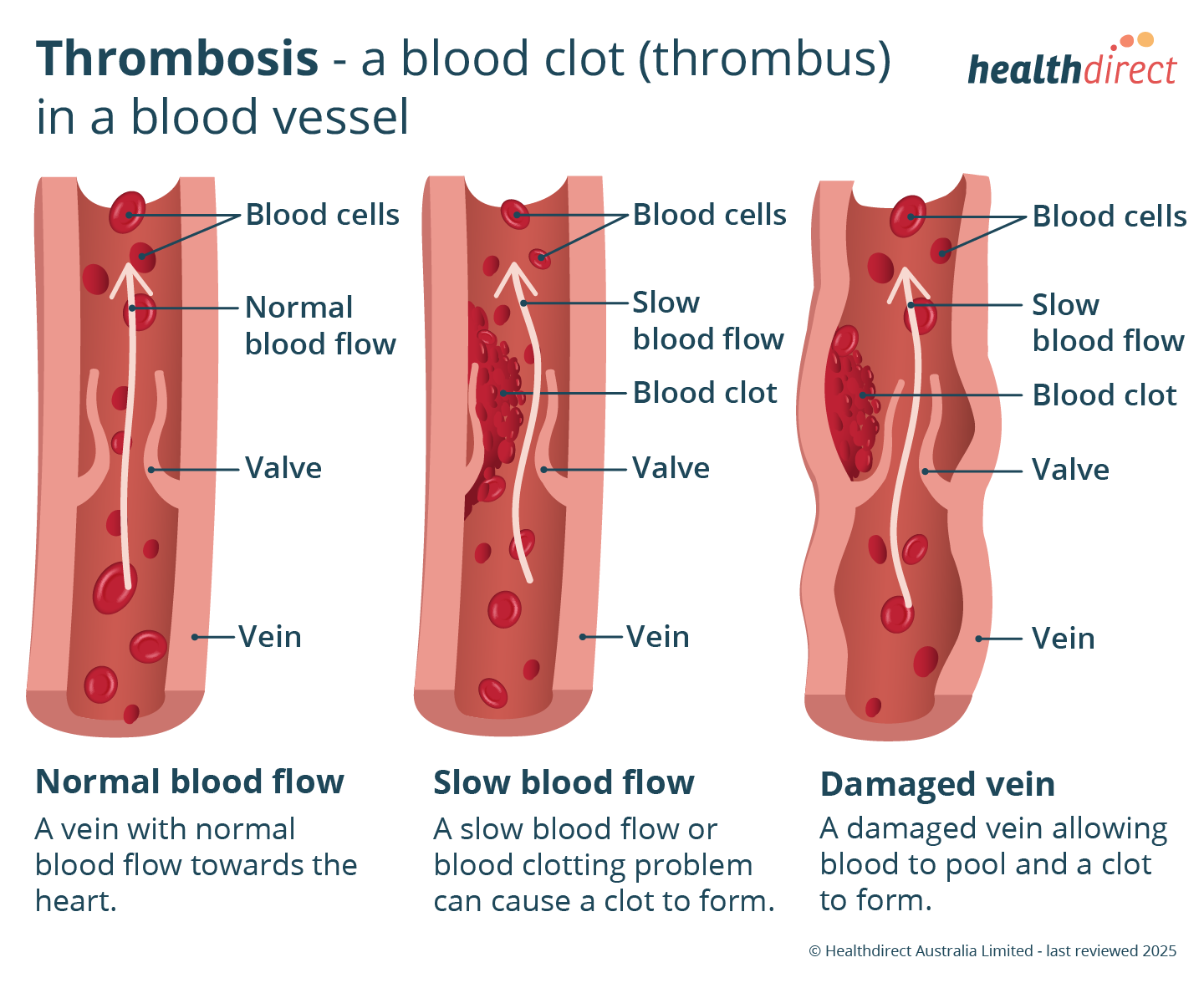
A blood clot in a blood vessel (thrombus) can happen when:
- your blood starts to clot more easily
- there is damage to the wall of the blood vessel
- there are changes in how your blood flows
Blood flow in your leg veins can slow down if you sit or lie still for a long time.
Often, a combination of things leads to a blood clot.
What can increase my risk of blood clots?
You are more likely to develop a DVT if:
- you've had recent surgery or an injury, especially a leg injury
- you've had a blood clot before
- you have a blood disorder or other condition that makes clotting more likely
- you have a family history of blood clots
- you smoke
- you stop moving around for a long period of time (for example, if you are in hospital or on a long-haul flight)
Other factors that can increase your risk of a DVT are:
- having cancer
- being pregnant or having recently given birth
- taking some types of hormonal contraception (birth control) or hormone replacement therapy that contain oestrogen
Having atherosclerosis (a build-up of cholesterol and other material in the walls of your arteries) increases your risk of blood clots that can cause heart attack and stroke.
When should I see my doctor?
Blood clots can cause serious complications. See your doctor as soon as possible if you think you may have a blood clot.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How are blood clots diagnosed?
Your doctor will ask you about your symptoms, overall health and lifestyle. They will also examine you.
Tests that can help diagnose a blood clot will depend on your symptoms and the part of your body that's affected. Your doctor may recommend:
- blood tests, including a D-dimer test
- an ultrasound scan
- a CT scan
- an electrocardiogram (ECG)
How are blood clots treated?
Treatment for a blood clot will depend on its location.
One treatment for blood clots is anticoagulant medicines (blood thinners). These medicines stop blood clots from growing larger and prevent new clots from forming.
You may need to take blood thinners for several months or longer. Regular follow up is needed with your doctor to check that the treatment is working.
Sometimes blood clots are treated with a medicine or procedure to:
- dissolve the clot
- prevent the clot from breaking up and travelling to your lungs, heart or brain
If you have a DVT, compression stockings may help with your symptoms and improve the blood flow in your legs.
If you have a heart attack, stroke or pulmonary embolism, you will need to have emergency treatment in hospital.
Can blood clots be prevented?
Some conditions or activities can put you at increased risk of blood clots. Your doctor may recommend medicines or other treatments to reduce your risk of blood clots.
You can also help lower your risk by:
- maintaining a healthy weight
- getting enough physical activity
- not smoking or vaping
Blood clot prevention when travelling
Long-distance travel can increase your risk of getting a DVT. To reduce your risk of blood clots during long-distance travel, try:
- getting up and moving about as much as possible
- doing foot exercises to help improve blood flow in your legs
- drinking plenty of fluids (but avoid alcohol)
Ask your doctor about whether compression stockings are a good idea when travelling.
Lifestyle measures to help prevent heart attack and stroke
To reduce your risk of conditions such as heart attack and stroke, your doctor may recommend lifestyle measures. These can include:
- eating a healthy diet
- maintaining a healthy weight
- getting enough physical activity
- not smoking
- reducing your alcohol intake
- reducing stress
Resources and support
Thrombosis Australia has more information on blood clots (thrombosis).
The Heart Foundation and Stroke Foundation have information on heart attack and stroke, including information in languages other than English.
If you want to know more about blood clots or need advice on what to do next, you can call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2025















