Pulmonary embolism
If you or someone else is having trouble breathing or chest pain, call triple zero (000) and ask for an ambulance.
Key facts
- A pulmonary embolism (PE) is a blood clot in your lung.
- The blood clot usually starts in a deep vein in your leg and travels to a blood vessel in your lung.
- Symptoms can include chest pain, trouble breathing and coughing up blood.
- The main treatment for a pulmonary embolism is blood-thinner medicines.
- There are things you can do to reduce your chances of having a PE.
What is a pulmonary embolism?
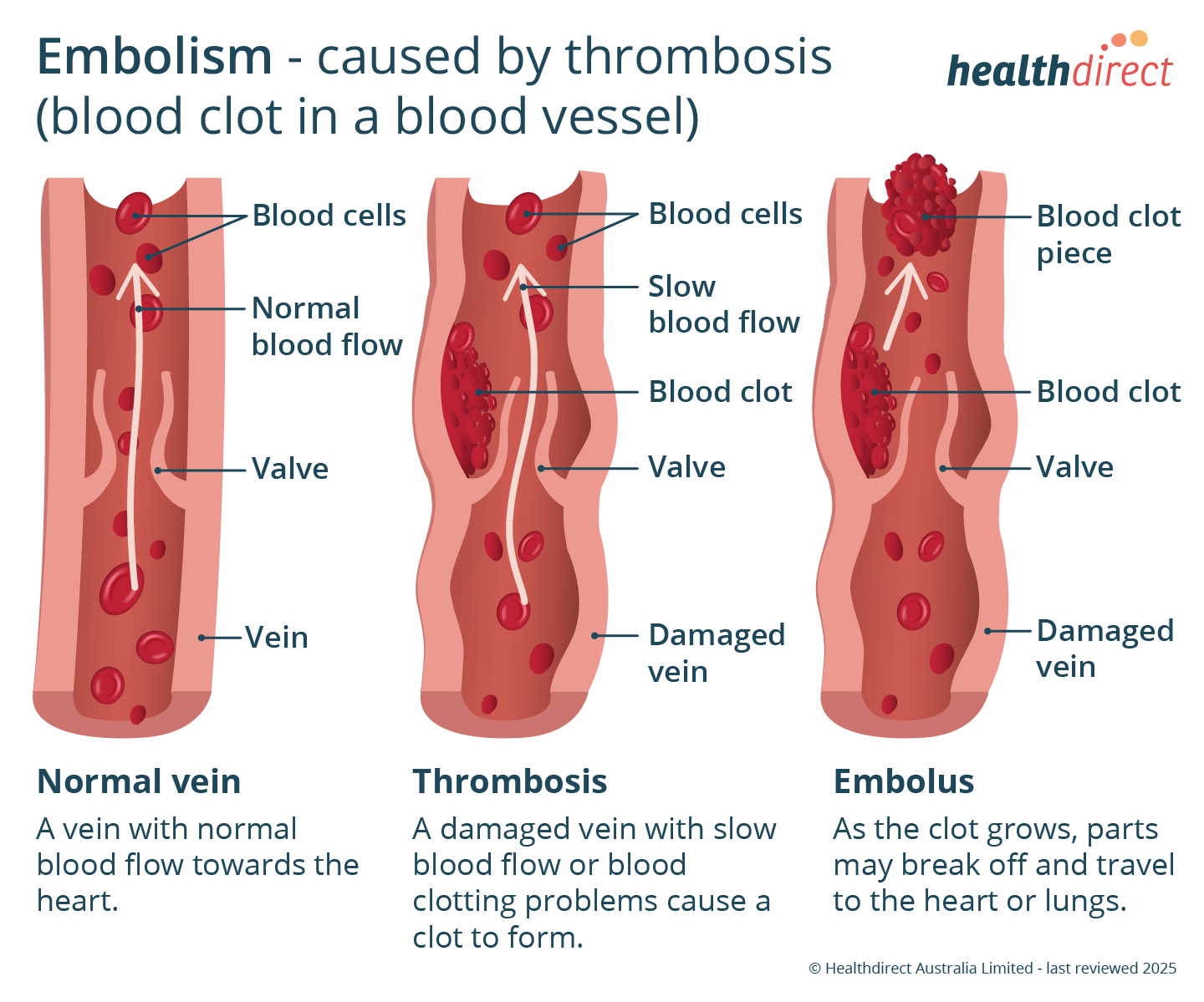
A pulmonary embolism is when a blood clot gets stuck in a blood vessel in your lung.
A blood clot in a blood vessel (artery or vein) is called a thrombus. An example of this is a deep vein thrombosis (DVT).
DVTs most often affect your legs. But they can occur elsewhere in your body, such as your arms or abdomen (tummy).
A pulmonary embolism can happen if part of a DVT breaks off and travels through your bloodstream to your lungs.
What are the symptoms of a pulmonary embolism?
The symptoms of a pulmonary embolism include:
- sudden or worsening breathlessness
- chest pain, which may be worse with deep breaths
- heart palpitations
- fast breathing and heart rate
- cough or coughing up blood
- fainting or lightheadedness
If you have these symptoms, go to your nearest emergency department or call 000 for an ambulance.
You may also have swelling, redness and pain in your leg. These are signs of a deep vein thrombosis (DVT).
What causes a pulmonary embolism?
The most common cause of a PE is a blood clot which has come from a deep vein thrombosis (DVT).
You are more likely to get a DVT if you:
- have a genetic (inherited) condition that causes blood clotting problems
- have had major surgery, for example a hip or knee replacement
- have been badly injured, such as a leg fracture
- have a severe illness such as cancer or heart failure
- are taking certain medicines containing oestrogen, such as the combined oral contraceptive pill
- are pregnant or have recently had a baby
- have had a pulmonary embolism or a DVT before
Some other risk factors for a DVT and pulmonary embolism include:
- being immobile (not moving), such as if you are recovering from illness, or travelling on long-haul flights
- older age
- obesity
- smoking
When should I see my doctor?
A pulmonary embolism is a serious condition. It can be life-threatening if not treated quickly. If you think you may have a PE, you should see a doctor straight away.
Call triple zero (000) for an ambulance if you:
- are having trouble breathing
- have chest pain
- have heart palpitations
- feel faint
- cough up blood
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is a pulmonary embolism diagnosed?
Your doctor will ask you about your symptoms and risk factors. They will examine you. Your doctor will check your vital signs, including your pulse and blood pressure.
You will need to have some initial tests, which may include:
- a D dimer blood test
- other blood tests
- a chest x-ray
- an electrocardiogram (ECG)
- an ultrasound scan of your legs to look for a DVT
You may have a scan used to diagnose a pulmonary embolism called 'computed tomography pulmonary angiography' (CTPA). This test looks for a blood clot in your lung.
A ventilation/perfusion scan (V/Q scan) is another test for PE. This scan uses a radioactive substance to find areas in your lungs where air and blood flow are mismatched because of a blood clot.
How is a pulmonary embolism treated?
If you have a PE, you will need initial treatment in hospital.
The main treatment is anticoagulant medicine (blood thinners). These medicines reduce further blood clotting. You might take tablets or have injections.
Some people need to have medicines called thrombolytics. These are used to break down and dissolve the blood clot. Sometimes a surgical procedure to remove the blood clot is needed.
What should I expect after a pulmonary embolism?
You may need to continue to take blood thinners for several months or more.
You will need regular follow up with your doctor.
If you are on warfarin, follow your doctor's instructions carefully as there can be risks of bleeding if the dose is not right for you.
What are the complications of pulmonary embolism?
A large pulmonary embolism is serious, and can cause:
- heart problems
- lung and breathing problems
- cardiac arrest and sudden death
Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare ongoing complication of pulmonary embolism. The main symptom is breathlessness when you move about.
If you have had a pulmonary embolism or a DVT, you are more likely to have another one later.
Can pulmonary embolism be prevented?
There are some steps you can take to help prevent DVTs and pulmonary embolism.
If you are having surgery or need to stay in hospital, you may need to:
- take blood-thinner medicines
- wear compression stockings if your doctor has recommended them
- use an inflatable compression device on your legs
- walk around as soon as possible after surgery
- move your feet and legs often if you are unable to walk around
- stay hydrated
If you are travelling for hours (for example, on planes or trains), remember to:
- get up to walk around every 1 or 2 hours
- do exercises like calf stretches or heel lifts
- drink plenty of water
- avoid alcohol or caffeine as these can add to dehydration
- wear compression stockings if you have other DVT risk factors
Other general things you can do to help prevent a DVT and PE are:
- quitting smoking
- getting regular physical activity
- maintaining a healthy weight
Resources and Support
Find out more about pulmonary embolism at Thrombosis Australia.
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2025












