Shingles
Key facts
- Shingles is an infection that causes a painful, blistering rash.
- It is most common in people over 50 years.
- Shingles can be treated with antiviral medicine.
- There is a vaccine to help prevent you from getting shingles.
- To help stop the spread of shingles, avoid direct skin contact and cover any sores that aren't under clothing.
What is shingles?
Shingles is a viral infection that causes a painful, blistering rash.
What are the symptoms of shingles?
The initial symptoms of shingles are:
- an area of sensitive skin with burning pain, tingling or itching
- sensitivity to light
- headache
- tiredness
Rash

About 2 to 3 days after the first symptoms, a rash will appear on sensitive skin. This rash usually appears on one side of your body around a skin nerve (called a dermatome).
At first, the rash consists of painful red bumps. These bumps quickly develop into fluid-filled blisters, which can be painful and itchy. These blisters will burst and then heal, forming a crusty surface over 2 weeks.
Shingles rash can affect your:
- face
- chest
- back
- abdomen (tummy)
- pelvis
The rash usually lasts for around 10 to 15 days, but it can take several weeks to settle.

CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes shingles?
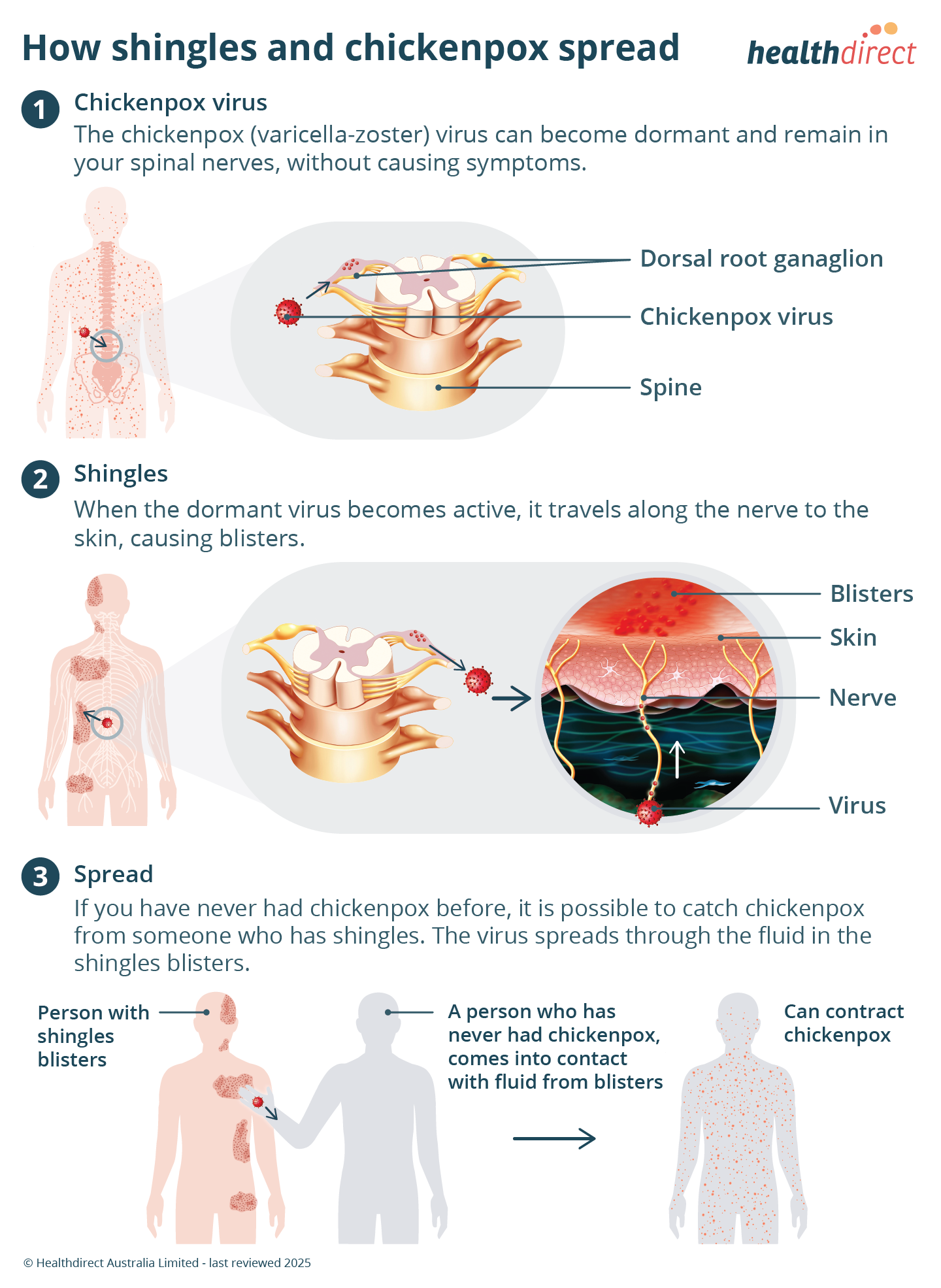
Shingles is caused by the reactivation of the varicella-zoster virus, which is the same virus that causes chickenpox.
After having chickenpox, the virus stays in the nerve cells of your body but is not active. Shingles occurs when the virus becomes active again usually many years later.
Although shingles often occurs for no known reason, the virus may be reactivated by:
- stress
- illness
- a weakened immune system (immunosuppression)
- older age
- trauma
- radiotherapy
Who can get shingles?
You can only get shingles if you have had chickenpox. Some people get chickenpox with only mild symptoms.
Shingles can happen at any age. The risk of shingles is higher in people:
- aged over 50 years
- with a weakened immune system
- who had chickenpox in their first year of life
About 1 in 3 people will develop shingles at some point in their life. Most people get shingles only once. But sometimes, especially if you have a weakened immune system, you might get repeat infections.
When should I see my doctor?
See your doctor if you have any symptoms of shingles.
Be sure to see your doctor as soon as possible if you have symptoms of shingles and:
- are pregnant
- have a weakened immune system
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is shingles diagnosed?
To diagnose shingles, your doctor will ask you about your symptoms and examine your rash. They may test fluid from your blisters and refer you for a blood test. This can confirm if your rash is caused by shingles.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is shingles treated?
There is no cure for shingles but, starting antiviral medicines within 3 days of the rash appearing can reduce the severity of your symptoms and your risk of complications.
Your doctor can prescribe antiviral medicine if you need it. If you are pregnant, talk to your doctor about whether antivirals are right for you.
Over-the-counter medicines can be used for pain relief, such as:
If over-the-counter medicines are not enough to manage your pain, your doctor may prescribe other medicines.
Managing shingles rash
There are several things you can do to help manage the condition.
Be sure to keep your rash dry and clean. After a bath or shower, dry your rash gently. Try not to scratch your rash, as this can cause an infection or scarring.
You can reduce the discomfort from your rash by:
- wearing loose fitting clothes
- using a cooled towel on the affected area
If possible, cover your rash, to avoid spreading the virus to other people. Use a non-stick dressing if the area isn't covered by light clothing.
Avoid antibiotic creams, gels, and adhesive (sticking) plasters or bandages on the blisters. These may slow down the healing process.
What are the complications of shingles?
Shingles usually gets better without long-term problems but some people may develop complications.
If you have shingles rash and it becomes infected, you may need to take antibiotics. A rare complication may include scarring from bacterial infection, and post inflammatory hypopigmentation — a loss of skin colour.
Shingles occurring in the eye area could result in temporary or permanent vision loss. If you do have shingles in your eye, your doctor may refer you to an ophthalmologist (eye specialist) for treatment.
Shingles can also cause facial drooping and Ramsay Hunt Syndrome. Visit your doctor if you have symptoms of Ramsay Hunt syndrome, which include:
- rash around the ear
- earache
- hearing loss
- dizziness
- difficulty moving your face muscles
Post-herpetic neuralgia
For around 1 in 10 people, the pain and tingling of shingles can last for months or even years. This is called post-herpetic neuralgia, and is more common in people over 50 years of age.
Can shingles be prevented?
Getting vaccinated against shingles reduces your chance of developing the condition. The shingles vaccine is recommended for:
- everyone aged 50 years and over
- people aged 18 years or older with a weak immune system
- people over 50 years who have contact with someone who has a weak immune system
People who have a weakened immune system includes people who:
- have HIV (human immunodeficiency virus) or AIDS (acquired immunodeficiency syndrome)
- are having cancer treatment
- have had an organ transplant or bone marrow transplant
- are receiving other medical treatment that affects their immune system
Vaccination does not guarantee that you won't get shingles, but it will reduce your chance of developing the condition.
The vaccine used to protect you against shingles is not the same as the vaccine used to protect against chickenpox. Read more about the chickenpox vaccine.
What are the recommendations for the shingles vaccine?
Vaccination is your best protection against shingles.
About the shingles vaccine
At what age is vaccination recommended?
The Australian Immunisation Handbook recommends shingles vaccination for specific groups including:
- people aged 50 years and over
- immunocompromised people aged 18 years and over
- people aged 50 years and over who live in the same household as someone who has a weakened immune system
How many doses?
2 doses
How is the vaccine administered?
The vaccine is given by injection.
Is it free?
Shingrix is free for:
- people aged 65 years or older
- Aboriginal and Torres Strait Islander people aged 50 years or older
- immunocompromised people aged 18 years or older with certain medical conditions
For everyone else, there is a cost for this vaccine.
Common side effects
The vaccine is safe. Side effects may include:
- pain, redness, swelling or itching where the needle went in
- headache
- tiredness
The Department of Health, Disability and Ageing has information on Zostavax, which is no longer available. People who have received Zostavax can still receive Shingrix.
Talk to your doctor about what is best for you. Ask your doctor about other vaccines you may need based on your situation or location.
LOOKING FOR A MEDICINE? — To search by brand name or active ingredient, use the Medicines information search feature.
How is the spread of shingles prevented?
You can’t catch shingles from someone who has shingles. You can get chickenpox from someone who has shingles if you have never had chickenpox.
Shingles is a nationally notifiable disease. If you are diagnosed with shingles, your doctor will tell your local public health authority.
The virus spreads if you have contact with fluid from the blisters. It is also spread by using or touching bedding, clothing or towels used by the person with shingles.
Unlike chickenpox, the shingles virus does not usually spread by coughing and sneezing. Cover the shingles blisters with a dressing to help reduce the risk of passing the virus to others. Once the blisters crust over, the person is no longer infectious.
If you have shingles, avoid contact with people who may be more at risk.
Be sure to wash your hands well and practise good hygiene.
Resources and support
For more information on immunisation in Australia, you can check:
If you want to know more about shingles you can call the healthdirect helpline on 1800 022 222 to speak with a registered nurse, 24 hours, 7 days a week (known as NURSE-ON-CALL in Victoria).
Languages other than English
The National Immunisation Program has an adult vaccinations consumer fact sheet available in many community languages.
Information for Aboriginal and/or Torres Strait Islander peoples
For more information about immunisation for Aboriginal and/or Torres Strait Islander people, visit the Department of Health, Disability and Ageing website.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2025


















