Rhabdomyolysis
Seek medical attention urgently if you have symptoms of rhabdomyolysis — muscle pain, muscle swelling, muscle weakness and dark urine.
Key facts
- Rhabdomyolysis is a serious condition caused when your muscle cells breakdown and their contents enter your bloodstream.
- Rhabdomyolysis is caused by many things, such as intense exercise, illegal drugs, alcohol, some medicines, injuries and illnesses.
- It’s important to get treatment early to avoid life threatening complications.
- Acute kidney injury is a complication of rhabdomyolysis.
- You may need to have fluids through an IV drip in hospital, medicines, surgery or dialysis to treat rhabdomyolysis.
What is rhabdomyolysis?
Rhabdomyolysis is the condition caused when your muscle cells breakdown. The contents of these cells are released into your bloodstream. It leads to muscle weakness, pain and swelling.
When your muscle tissue is seriously injured, it breaks down releasing the chemicals from the muscle into your blood.
This can change the balance of electrolytes (minerals and salts) in your body, which can lead to serious problems with your heart and other organs. It can also reduce your kidney function and cause kidney failure.
What are the symptoms of rhabdomyolysis?
The symptoms of rhabdomyolysis will depend on the cause, but include:
- muscle pain or swelling
- muscle weakness
- fatigue (tiredness)
- dark red to brown urine (wee)
- fever
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
When should I call an ambulance or go to the emergency department?
Seek medical attention urgently if you have symptoms of rhabdomyolysis —muscle pain, muscle swelling, muscle weakness and dark urine.
Symptoms of rhabdomyolysis may not start for hours or days after your muscle injury.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
What causes rhabdomyolysis?
Rhabdomyolysis is caused by an injury to your muscle tissue. This can be caused by many things, including:
- trauma and exercise
- medicines and other substances
- illness
Trauma and exercise causes of rhabdomyolysis include:
- trauma or crush injuries, for example, from a car accident
- extreme muscle use, for example, running marathons
- being immobile for a long time
- envenomation from multiple insect bites or stings or from a snake bite
Medicine and other substance causes of rhabdomyolysis include:
- taking illegal drugs such as cocaine, amphetamines or ecstasy
- a rare side effect of some medicines, such as statins (cholesterol-lowering drugs) or diuretics
- drinking too much alcohol
- carbon monoxide poisoning
- being bitten or stung by wasps, hornets or snakes
Illness causes of rhabdomyolysis include:
- some genetic conditions, such as muscular dystrophy
- autoimmune conditions, such as dermatomyositis and polymyositis
- very high body temperature, such as hyperthermia or heat stroke
- having a seizure
- infections
How is rhabdomyolysis diagnosed?
Your doctor will ask you about your symptoms and examine you. You will also need blood tests and urine tests. Rhabdomyolysis is often diagnosed in hospital.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is rhabdomyolysis treated?
Rhabdomyolysis is treated in hospital by giving you fluids through an intravenous (IV) drip. The fluids help prevent acute kidney injury.
Your doctors will closely check the electrolyte (mineral and salt) balance in your blood.
In rare cases, you may need dialysis. A dialysis machine filters your blood to remove the harmful chemicals and high levels of electrolytes. The machine then returns the filtered blood back to your veins.
Other treatments will depend on the cause of your rhabdomyolysis.
Early diagnosis and treatment of rhabdomyolysis increases your chances of a full recovery.
What are the complications of rhabdomyolysis?
If not treated early, rhabdomyolysis can lead to complications, such as:
- changes in the electrolyte (mineral and salt) levels in your blood which can lead to an arrhythmia (irregular heartbeat)
- kidney injury
- bleeding and clotting problems
- compartment syndrome
If you have compartment syndrome you may need urgent surgery to avoid more muscle death or nerve damage.
Can rhabdomyolysis be prevented?
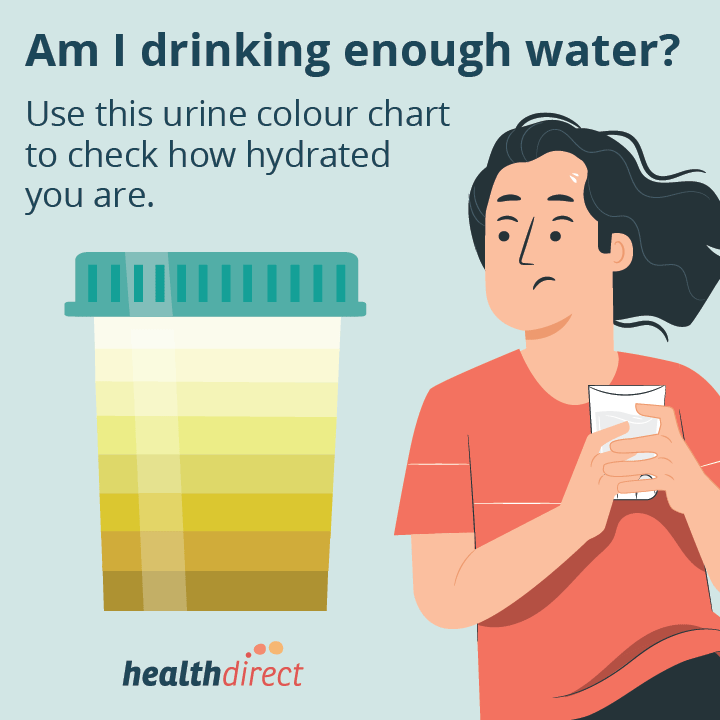
You can lower your chance of developing rhabdomyolysis by staying hydrated.
Talk with your doctor or pharmacist about any medicines you take that may increase your chance of developing rhabdomyolysis.
You can’t prevent all causes of rhabdomyolysis, such as when it’s caused by an underlying health condition or an accident.
You can prevent exercise-induced rhabdomyolysis by slowly building up resistance training.
Read more on how to start strength training in a safe way.
Resources and support
If you are concerned about muscle pain, but it is not an emergency, call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with you 24 hours a day, 7 days a week.
NPS Medicinewise has a fact sheet on statin safety.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2025









