Dialysis
Key facts
- Dialysis is a treatment that removes extra fluids and waste products from your blood if your kidneys aren't functioning well enough.
- There are 2 different types of dialysis — haemodialysis and peritoneal dialysis
- During haemodialysis, your blood runs through a machine and back into your body after it has been treated.
- Peritoneal dialysis uses fluid pumped into the lining of your belly (the peritoneum) to help filter your blood.
- You can still live a full and productive life if you are on dialysis.
What is dialysis?
Dialysis is a treatment that removes extra fluids and waste products from your blood if your kidneys aren't functioning well enough.
Your kidneys act as filters for your body. They remove waste and extra fluid from your blood and get rid of it via your urine (wee). If your kidneys are not working properly, waste and fluid can build up in your blood. This can severely impact your health.
When is dialysis needed?
Dialysis is needed in cases of severe kidney failure.
Kidney disease can be short-term (acute kidney injury) or lifelong (chronic kidney disease).
Acute kidney injury happens when your kidneys do not work temporarily, for less than 3 months. This can happen suddenly due to a serious illness or accident. You may need dialysis treatment for a short period of time to help your kidneys recover. Many people can recover from an acute kidney injury.
Chronic kidney failure is when your kidneys' ability to work is affected for more than 3 months. Dialysis is only usually needed when your kidneys are severely damaged. At this point you may find it hard to manage your normal activities. You will need dialysis treatment for the rest of your life unless you have a kidney transplant, or you choose renal supportive care instead.
What are the different types of dialysis?
There 2 main types of dialysis are haemodialysis and peritoneal dialysis.
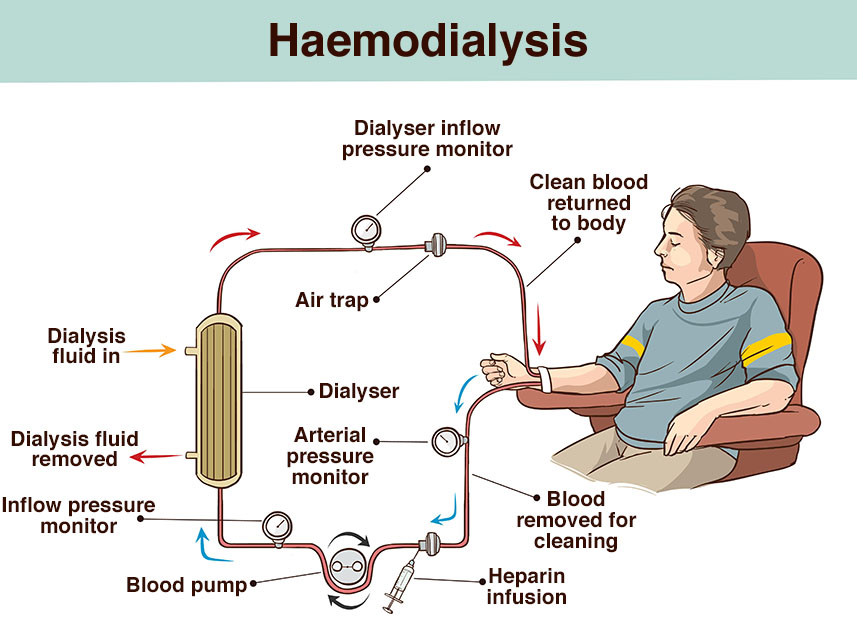
Haemodialysis
Haemodialysis treatment uses a special machine called a 'dialyser'.
You will be connected to a dialyser through a needle usually in your arm, neck or leg. The dialyser filters the blood from your body and removes waste and extra fluid, before pumping it back into your body.
You will usually need to have haemodialysis 3 days a week. Each treatment lasts for 4 to 5 hours.
You can have haemodialysis at a special clinic or sometimes at home.
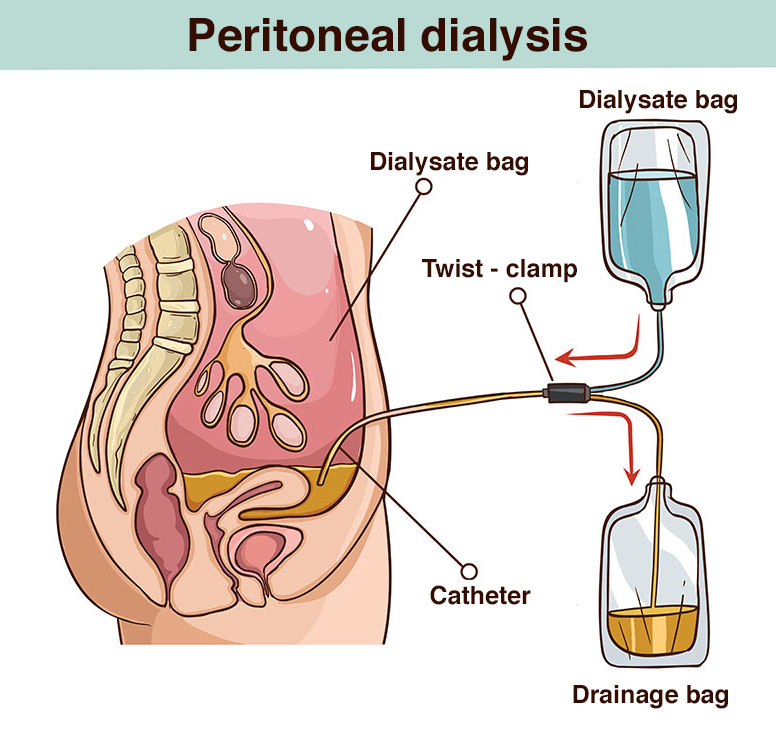
Peritoneal dialysis
Peritoneal dialysis uses the lining in your abdomen (belly) — called the peritoneum — to act as a natural filter for your blood.
When you have peritoneal dialysis, a fluid is pumped into a space in your abdomen called the peritoneal cavity. The fluid enters and leave through a catheter. The catheter is a thin, soft tube, about 30cm long, that stays in place all the time. Waste from your blood moves into the fluid in your peritoneal cavity. The fluid is then removed from your body via the catheter.
Peritoneal dialysis needs to be done daily, either:
- manually (continuous ambulatory peritoneal dialysis) about 4 times during a 24-hour period, each session lasting about 30 – 40 minutes
- by a machine (automated peritoneal dialysis), overnight for 8 – 10 hours
Many people find they can fit peritoneal dialysis into their lifestyles.
Both haemodialysis and peritoneal dialysis are usually free in Australia for Medicare card holders. If you have dialysis in your home, there may be some expenses. You may be eligible for financial support from the government.
Living with dialysis
Starting dialysis can significantly affect your life. It is very important that you do not miss a dialysis session. However, you can still have an active life, with some adjustments to your work and home life.
The type of dialysis that is right for you will depend on:
- your lifestyle
- your vision
- your dexterity (coordination and mobility)
- whether you have a carer
- where you live
Treatment with dialysis allows most people to continue to:
- be physically active
- maintain a balanced diet
- keep socially engaged
- have intimate relationships
What is renal supportive care?
Renal supportive care is personalised care that helps to manage symptoms of kidney failure so that you can enjoy a good quality of life.
Supportive care is available to everyone with kidney failure.
A multidisciplinary care team made up of specialist doctors, nurses and allied health professionals will look after you. They will support you to manage:
- your medicines
- your diet
- symptoms such as pain, itch, and nausea
- decisions and planning for end-of-life care
Supportive care can also be an alternative to dialysis or kidney transplantation.
You might choose supportive care if you:
- do not want dialysis treatment
- cannot have dialysis treatment
- choose to stop dialysis treatment
Read more about coping with learning you have a terminal illness.
Resources and support
You can read more about kidney disease and dialysis on the Kidney Health Australia website.
You can call Kidney Health Australia on 1800 454 363 to get support around your kidney health.
You can also call the healthdirect helpline on 1800 022 222. A registered nurse is available 24 hours a day, 7 days a week.
Do you prefer to read in languages other than English?
Kidney Health Australia has many factsheets about your kidneys in different community languages.
Looking for information for Aboriginal and/or Torres Strait Islander people?
Kidney disease is more common amongst Aboriginal and Torres Strait Islander people and Kidney Health Australia has a helpful factsheet explaining how you can keep your kidneys healthy and strong.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2024













