Abdominal Surgery for Crohn's disease
What is Crohn’s disease?
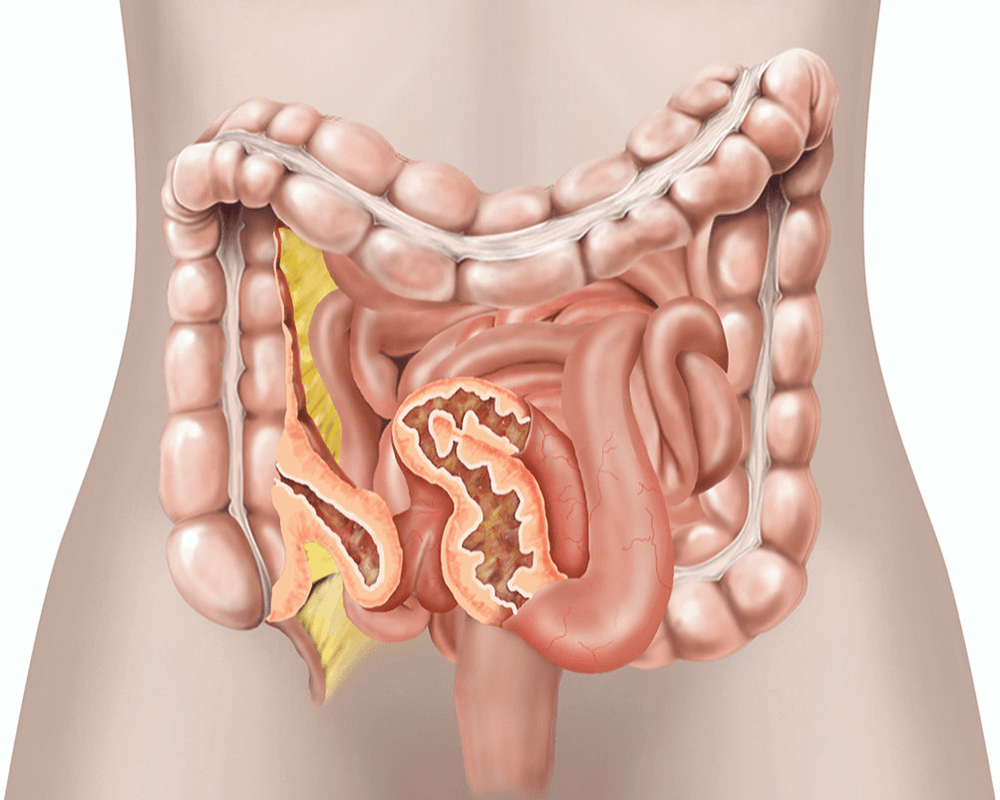
Crohn’s disease causes inflammation of your bowel. The disease most often affects the end part of your small bowel, called the terminal ileum. However, it can affect any part of your bowel.
Crohn’s disease causes your bowel wall to thicken, which can block food from passing through. The affected area of your bowel can also fail to absorb nutrients from your food.
What are the benefits of surgery?
Your symptoms should improve. Your doctor may also be able to reduce or stop your medication.
Are there any alternatives to surgery?
Inflammation can be treated using medication such as mesalazine, steroids, azathioprine and infliximab. These have side effects and your doctor will discuss them with you.
Sometimes a narrowing of your bowel can be stretched by a procedure that uses a flexible telescope and a balloon dilator.
What does the operation involve?
The operation is performed under a general anaesthetic.
Your surgeon will make a cut on your abdomen and remove the diseased part of your bowel.
Your surgeon will usually join the ends of your bowel back together. If they are unable to join the ends of your bowel, they will make a colostomy or ileostomy (your bowel opening onto your skin).
How can I prepare myself for the operation?
If you smoke, stopping smoking now may reduce your risk of developing complications and will improve your long-term health.
Try to maintain a healthy weight. You have a higher risk of developing complications if you are overweight.
Regular exercise should help to prepare you for the operation, help you to recover and improve your long-term health. Before you start exercising, ask the healthcare team or your GP for advice.
Speak to the healthcare team about any vaccinations you might need to reduce your risk of serious illness while you recover. When you come into hospital, practise hand washing and wear a face covering when asked.
What complications can happen?
General complications of any operation
- bleeding
- infection of the surgical site (wound)
- allergic reaction to the equipment, materials or medication
- acute kidney injury
- developing a hernia in the scar
- blood clot in your leg
- blood clot in your lung
- chest infection
- difficulty passing urine
Specific complications of this operation
Keyhole surgery complications
- damage to structures such as your bowel, bladder or blood vessels
- developing a hernia near one of the cuts used to insert the ports
- surgical emphysema
- gas embolism
Complications of surgery for Crohn’s disease
- anastomotic leak
- continued bowel paralysis
- damage to other structures inside your abdomen
- injury to your bowel
- tissues can join together in an abnormal way
- compartment syndrome causing pain and damage to your legs
- Death. The risk is less the fitter you are.
Consequences of this procedure
- pain
- unsightly scarring of your skin
How soon will I recover?
You should be able to go home after 3 to 10 days.
It may take up to 3 months for you to recover fully. Most people feel much better after the diseased part of their bowel has been removed.
Regular exercise should help you to return to normal activities as soon as possible. Before you start exercising, ask the healthcare team or your GP for advice.
Crohn’s disease sometimes comes back and affects another part of your bowel or a part near to where the join was made.
Summary
Crohn’s disease causes inflammation of your bowel. Surgery is usually recommended if medication fails to improve your symptoms.
IMPORTANT INFORMATION
The operation and treatment information on this page is published under license by Healthdirect Australia from EIDO Healthcare Australia and is protected by copyright laws. Other than for your personal, non-commercial use, you may not copy, print out, download or otherwise reproduce any of the information. The information should not replace advice that your relevant health professional would give you. Medical Illustration Copyright © Medical-Artist.com.
For more on how this information was prepared, click here.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2024















